

Lymphoedema
Lymphoedema develops through the accumulation of protein-rich fluid in the tissue. Lymphatic fluid (lymph, Latin: Lympha = clear water) cannot be removed sufficiently by an impaired lymphatic system and accumulates as a result. Lymphoedema can develop in all parts of the body but affects the legs in a majority of cases.
The lymphatic system
The lymphatic system runs through the whole body, usually parallel to the blood vessels. It is not a closed circuit, but rather a semi-open system.
As the most important element of the human immune system, it acts as a transport and waste removal system for substances such as protein, dietary fats, pathogens or cell debris. This lymphatic load cannot be broken down by the body in any other way. A disruption of the lymphatic system causes accumulation of fluid and thus visible and palpable swelling, that is, an oedema.
What is lymphoedema?
Definition of lymphoedema: This is an accumulation of lymphatic fluid in the tissue that causes a local swelling of the tissue. It is caused by a restricted transport capacity of the lymphatic system.
The most common causes of lymphoedema are previous conditions or treatments such as, for example, breast cancer surgery involving the removal of lymph nodes. Lymphoedema does not develop immediately following surgery. This often happens years later, i.e. with a long delay of the onset. A congenital disposition (e.g. an insufficient number of lymph vessels) is much more rare.
It can therefore happen that the condition is not immediately recognised as lymphoedema. During the time that passes without treatment, the lymphoedema can deteriorate and make later treatment more difficult.
In most cases, lymphoedema is not accompanied by pain but leads to severe swelling with tightness in the affected areas that often results in major restrictions in movement and further complications. Both women and men are affected by lymphoedema.
What types of lymphoedema are there?
Lymphoedema can be divided into two types based on different causes:
Primary lymphoedema
Primary lymphoedema can develop immediately after birth or during the course of your life. The causes for the disrupted lymphatic system in this case are:
- Congenital absence of lymph vessels
- Over or underdevelopment of lymph vessels and lymph nodes
- Hardening of lymph nodes
Secondary lymphoedema
Secondary lymphoedema is a lot more common than primary lymphoedema. There will always have been a preceding cause that resulted in damage or an impairment of the lymphatic system. Secondary lymphoedema can develop in any area of the body and can have a variety of causes.
Examples for causes of secondary lymphoedema:
- Injuries causing damage to lymphatic pathways or lymph nodes
- Surgical procedures requiring the removal of lymph nodes or sectioning of lymph vessels (e.g. breast cancer surgery)
- Inflammations due to viruses, bacteria, fungi, etc.
- Untreated chronic venous insufficiency
- Tumours, malignancies, radiation, infections, insect bites, etc.
Mixed forms of lymphoedema
In addition to the primary and secondary types of lymphoedema, mixed forms of oedema can also develop:
Phlebolymphoedema
Phlebolymphoedema almost exclusively develops on the legs. It is the consequence of a phlebological condition, i.e. a disorder of the cardiovascular system such as varicose veins or thrombosis. Due to increased pressure in the veins, more fluid is pressed out of the blood vessels into the tissue. If a temporary oedema that developed as a consequence of a venous disorder (phleboedema) remains untreated, the lymphatic system will become overloaded over time. The tissue hardens and phlebolymphoedema will develop.
Obesity-related lymphoedema
During advanced stages of pathological obesity, obesity-related lymphoedema can develop. This is usually symmetrical. The enlarged and increased number of fat cells apply pressure on the lymphatic system and impair its functionality. Lymph transport and the absorption of lymphatic fluid in the lymph nodes is obstructed. Furthermore, the increase of fatty tissue results in an inflammatory process that damages the lymph vessels. Based on this damage, the lymph vessels leak and fluid penetrates the surrounding tissue.
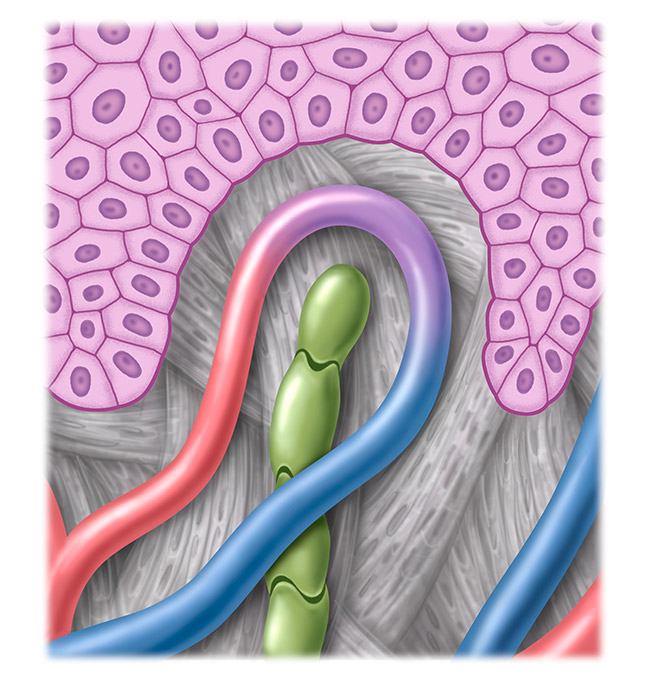
Healthy lymphatic system
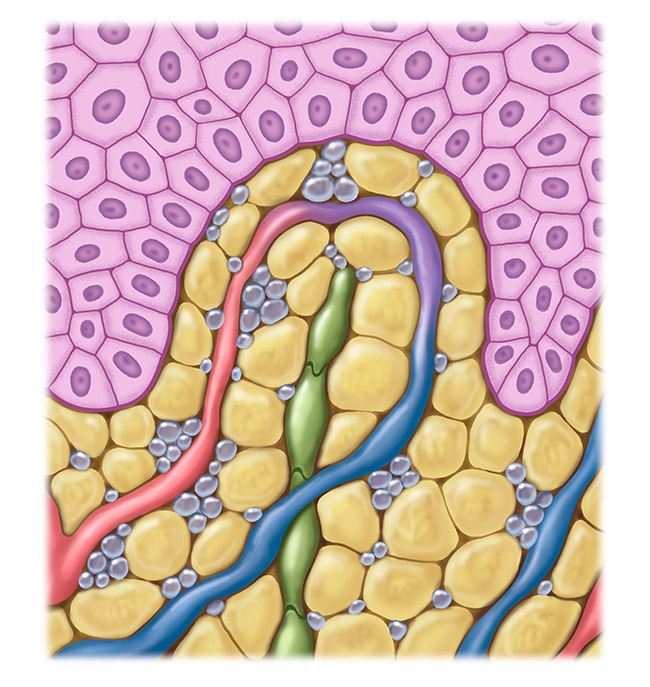
Affected lymphatic system
Lymphoedema symptoms
The symptoms of lymphoedema can be categorised into internally perceptible symptoms and externally visible symptoms. You can use the following signs to identify whether you are potentially suffering from lymphoedema.
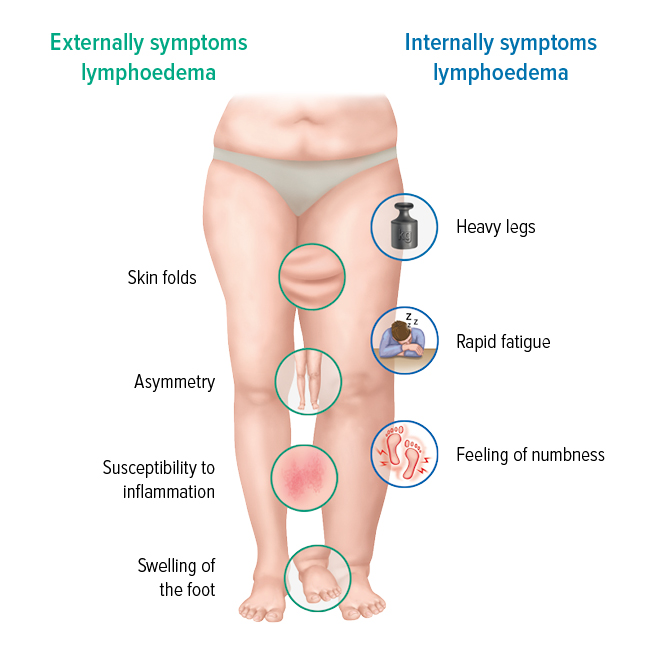
Externally visible symptoms
These signs are clearly evident on the affected parts and can, to a varying extent, have the following characteristics:
- Positive Stemmer’s sign
- Swelling of a limb that is not the same on both sides but asymmetrical (e.g. just one leg)
- The back of the foot or hand is generally swollen
- Skin discolourations and other skin changes
- Susceptibility to inflammations and skin irritations
- Clearly perceptible skin folds on the affected limbs
- Possible movement restrictions
Internally perceptible symptoms
In addition to the visible signs, there are other symptoms that could indicate lymphoedema:
- Tired, heavy limbs
- Feeling of tension and tightness
- Tingling or twinges
- Slight numbness of the affected body part
- Quicker fatigue of the affected leg or arm
If you notice one or more of the signs of lymphoedema, please consult a specialist for veins or lymph vessels. Early diagnosis has a positive effect on the progression of the condition.
Stemmer’s sign and thumb test
A positive Stemmer’s sign may indicate a leg lymphoedema. You can easily test this yourself.
- Try to lift the skin on your second toe with your index finger and thumb. If you can lift the skin and it is easy to hold on to, this is a negative Stemmer’s sign. In this case it is unlikely that you have lymphoedema.
- If you cannot lift the skin, this is a positive Stemmer’s sign, indicating that it is likely you have lymphoedema in the leg.
- Compare the skin folds on the second toes on both feet. On a foot with a positive Stemmer’s sign, this skin fold is significantly thicker.
If the swelling is on another part of the body, the thumb test can help. Press your thumb into the affected tissue for about 10 seconds! If the indentation does not disappear immediately, once you have removed the thumb, this would indicate lymphoedema.
A negative Stemmer’s sign does not always mean that lymphoedema can be excluded. If you have other symptoms, it is essential that you consult a specialist to examine the problem.
Differentiating lymphoedema and lipoedema
Lipoedema is a painful fat distribution disorder that also causes growth in the circumference of limbs. They are sometimes mistaken for one another, but lipoedema and lymphoedema are different in many respects. To illustrate the differences between the two conditions, lymphoedema and lipoedema, we have drawn up a comparison of the most important distinguishing criteria. This makes it easier for you to understand a potential diagnosis.
| LYMPHOEDEMA | LIPOEDEMA | |
| Appearance of the oedema | asymmetrical & symmetrical | only symmetrical |
| Pain (pressure, touch, etc.) | no | yes |
| Infection of the upper dermis and superficial lymphatics (Erysipelas) | common | no |
| Swelling on back of foot and/or hand | yes | no |
Important: This self-check is not a replacement for seeing a medical specialist. It is crucial that you consult a medical specialist to obtain a correct diagnosis.
What are the stages of lymphoedema?
Lymphoedema can be divided into four stages, depending on severity. The stage also determines the type of treatment which should commence immediately upon diagnosis to counteract any spread or deterioration.
Stage 0 – latency stage

Stage 0 – latency stage
- Diagnosed damage to the lymphatic system
- Oedema not (yet) visible
Stage I – spontaneously reversible stage

Stage I – spontaneously reversible stage
- Soft swelling
- Elevation results in a reduction of the oedema
- Finger pressure leaves a visible indentation
Stage II – not spontaneously reversible stage

Stage II – not spontaneously reversible stage
- Hardening of the connective tissue
- Elevation does not result in a reduction of the oedema
- Creating an indentation with the finger is scarcely possible
Stage III – irreversible stage

Stage III – irreversible stage
- The volume of the affected body part has increased dramatically
- Hardened skin with skin changes
- Severely restricted mobility
The treatment concept for lymphoedemas
Complex decongestive therapy (CDT) is the only treatment method that has been proven to contribute to an improvement of the condition or counteract a possible deterioration of lymphoedema. In the first phase of CDT, the tissue is decongested as much as possible. This is accomplished by manual lymph drainage (MLD), daily if possible, and compression treatment tailored to the lymphoedema stage using adjustable compression wraps (ACW) or compression bandages. In the second phase, the goal is to maintain the decongested condition using MLD and an individually manufactured flat knit compression garment (Juzo Expert or Juzo Expert Strong). Skin care, decongestion exercises and the necessary degree of personal initiative on the part of the patient are important for the entire treatment. Consistent and sustained treatment is the only way of reducing the severity of lymphoedema and maintaining this success in the long term.
Surgical methods
- Partial or complete removal of the increased tissue resulting in a lower production of lymph (resection methods)
- Drainage of the lymphatic fluid from the lymphatic system via extra-anatomical ways e.g. by linking the lymph vessel and vein (drainage method)
- Linking blocked or interrupted sections of the lymphatic system e.g. by transplanting lymphatic pathways and lymph nodes (reconstructive methods)
All of these measures and methods are subject to highly special conditions and requirements and their benefits and risks must always be assessed.
What complications can occur?
If lymphoedema remains untreated or is treated inadequately or in the wrong way, skin abnormalities, hardening of the tissues and other complications can develop leading to additional problems.
The skin on the body parts affected by lymphoedema can dry out and become scaly. Protein that cannot be sufficiently transported away by the lymphatic system collects in the tissues. This can lead to inflammation. New connective tissue forms and the oedema consequently gets bigger and hardens (fibrosis).
Because the immune system of lymphoedema patients is impaired in the affected area, the organism is more prone to skin infections such as erysipelas or fungal infections (mycosis). These require immediate medical treatment.
